Non-Invasive ICP Monitoring for Hydrocephalus
DiaCeph Test directs perfect outcome in
2008 shunt revision: Read the
Shunt Selection Model case study. 
In 2008, Stephen Dolle, inventor of the DiaCeph Test and a CNS shunt user, used his DiaCeph Test and Shunt Selection Method to direct a successful shunt revision, after 16 years of poor outcomes by some of the best neurosurgeons around.
As a result of numerous inquiries, Stephen now offers DiaCeph shunt monitoring services & consults based on the DiaCeph Test method, and using his established paper forms & instructions. He is currently preparing a proposal to have the DiaCeph made into a mobile app for mobile phones. He also uses an array of current mobile health apps to help with daily living, management of headache, and for cognitive aids.
Imagination In Common with Albert Einstein
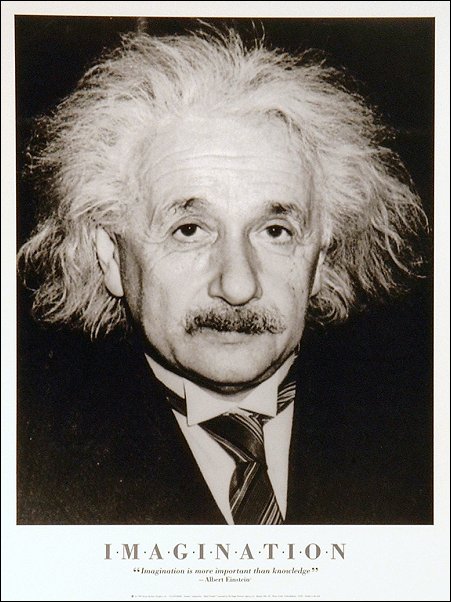 Stephen Dolle, the inventor of the
DiaCeph Test,
says he was driven by "imagination" and "need" in designing the DiaCeph Test,
much as were Albert Einstein, Henry Ford,
and others were in creating their inventions. With a strong background in
nuclear medicine imaging, and now living with hydrocephalus, he knew what was
needed and took it upon himself to first author a
special petition to the FDA in 1996, and then
follow it up with the design of the DiaCeph Test so that others too could live a
better life.
Stephen Dolle, the inventor of the
DiaCeph Test,
says he was driven by "imagination" and "need" in designing the DiaCeph Test,
much as were Albert Einstein, Henry Ford,
and others were in creating their inventions. With a strong background in
nuclear medicine imaging, and now living with hydrocephalus, he knew what was
needed and took it upon himself to first author a
special petition to the FDA in 1996, and then
follow it up with the design of the DiaCeph Test so that others too could live a
better life.
It was in 1996 after undergoing three CNS shunt revisions and being dissatisfied with the results, he Petitioned the Food & Drug Administration on problems he discovered with anti-siphon shunts. He collected scientific data and literature spanning more than 30 years in the care and treatment of hydrocephalus. Routine diagnostic tests were (and still) are not able to detect these. Higashi et. al. and many other neurosurgeons reported diagnostic difficulties with anti-siphon shunts, which Higashi's team termed "functional obstructions," not detectable through routine CT, MRI, and shunt malfunction tests. By contrast, the Food & Drug Administration, said such monitoring was not technologically possible per Petition Ruling Comments #3 and #7.
 Ongoing correspondence with FDA suggests that they
do not understand CNS shunt technology nor the critical role diagnostic testing
should play in their everyday use. CNS shunts are classified as Class II medical devices under the
FDA. Manufacturers are required to identify maintenance procedures for
their safe and efficacious use. It would seem, based upon
the rate of failure and diagnostic difficulties with CNS shunts, that manufacturers
have not met the troubleshooting requirements set forth in the Code
of Federal Regulations (CFRs) covering CNS shunts. Industry has merely passed on
the problem to user neurosurgeons, who are not in the technology business. In 1999, the FDA held a special one-day
International
STAMP Conference in Washington, D.C., to better address the issues Stephen raised in his
1996 Petition and other
correspondence. Stephen authored a
STAMP
Paper of Recommendations in support of this STAMP Conference. Stephen then requested
the FDA prioritize its goals
with CNS shunts in this
1999 Letter to
Larry Kessler, Ph.D., and Dept. Head of the STAMP Conference. Stephen
specifically noted the need for STAMP support of home shunt monitoring, but
Larry
Kessler's Response termed it "discretionary
technology." As of 2006, the FDA has failed to meet few if any of the consensus
positions as determined by STAMP.
Ongoing correspondence with FDA suggests that they
do not understand CNS shunt technology nor the critical role diagnostic testing
should play in their everyday use. CNS shunts are classified as Class II medical devices under the
FDA. Manufacturers are required to identify maintenance procedures for
their safe and efficacious use. It would seem, based upon
the rate of failure and diagnostic difficulties with CNS shunts, that manufacturers
have not met the troubleshooting requirements set forth in the Code
of Federal Regulations (CFRs) covering CNS shunts. Industry has merely passed on
the problem to user neurosurgeons, who are not in the technology business. In 1999, the FDA held a special one-day
International
STAMP Conference in Washington, D.C., to better address the issues Stephen raised in his
1996 Petition and other
correspondence. Stephen authored a
STAMP
Paper of Recommendations in support of this STAMP Conference. Stephen then requested
the FDA prioritize its goals
with CNS shunts in this
1999 Letter to
Larry Kessler, Ph.D., and Dept. Head of the STAMP Conference. Stephen
specifically noted the need for STAMP support of home shunt monitoring, but
Larry
Kessler's Response termed it "discretionary
technology." As of 2006, the FDA has failed to meet few if any of the consensus
positions as determined by STAMP.
The photo below is of Stephen in 1998 after completing the design of his DiaCeph Test and
using it to direct his
Feb. 1998 shunt revision. It took him 5 years to determine he had been
incorrectly implanted with a Delta shunt. Still without corrective surgery, it
caused him to pursue a series of algorithms that
enabled him to non-invasively determine what was wrong with his shunt - a method
later hailed by Dr. Eldon Foltz, of the University of California at Irvine, as
"the formula [he] had sought for years." The photo of Stephen as a
shunt
pioneer parallels similar efforts of the late John Holter.
years to determine he had been
incorrectly implanted with a Delta shunt. Still without corrective surgery, it
caused him to pursue a series of algorithms that
enabled him to non-invasively determine what was wrong with his shunt - a method
later hailed by Dr. Eldon Foltz, of the University of California at Irvine, as
"the formula [he] had sought for years." The photo of Stephen as a
shunt
pioneer parallels similar efforts of the late John Holter.
Upon completion and validation of the method, Stephen named it the "DiaCeph Test," meaning "dia" to diagnose and "ceph" having to do with the brain. Stephen's 17-year career in nuclear medical imaging and in math/physics provided critical knowledge in drafting the algorithms. The DiaCeph Test employs a sophisticated software design to run on PDAs and mobile phones, and connect to a PC or Internet network to display results. DiaCeph's proprietary protocol and algorithms non-invasively track shunt performance data and generate a diagnostic profile on the user-patient. Up to 15 separate states of shunt malfunction and hydrocephalus are assessed.
In 1999, the DiaCeph Test was featured in the Orange County Business Journal. A patent was issued in 2001, with a second patent optioned. Patent representation has been provided by the prestigious firm of Knobbe Martens Olsen & Bear. In 1997, AI monitoring and disease algorithms were very new. Today, new applications are on the rise in disease management (asthma, congestive heart failure, diabetes), hospital monitoring, and patient data mining.
In 2005, we introduced a tandem protocol that incorporates an ICP shunt tap along with DiaCeph monitoring, as described in Shunt Selection Model. Our paper includes comparative shunt data from Aschoff, et. al. at the University of Heidelberg. The tandem protocol is critical as it raises both tests' accuracy and reliability: corroborating DiaCeph data with widely recognized shunt tap/ICP assessments. One in-office ICP measurement can validate weeks and months of critical DiaCeph monitoring, and help the patient and family better realize its benefits. The DiaCeph Test already has a built-in logic processor to identify and resolve any "erroneous data" that might be mistakenly entered by a patient, guardian, or family member. But matching incident DiaCeph data to supine/upright manometer readings, further elevates DiaCeph's efficacy, while corroborating the ICP readings.
Widespread use of this tandem protocol can reduce the costs and risks associated with CT, MRI, in-office ICP taps, isotope imaging, and in-hospital monitoring. It can lead to fewer unnecessary shunt revisions, and render in-office shunt re-programming more accurate to the patient. We were able to match months of DiaCeph data monitoring with a single shunt/ICP evaluation. It widens DiaCeph's applications in 24/7 home monitoring, where only 48 hour ICU in-hospital monitoring provided such capability. With new interests in non-invasive monitoring, DiaCeph's applications are broad and economical.
Reliable shunt function remained a leading issue among shunt users, where programmable shunts (which comprise about 50% of all shunts) are prone to accidental reprogramming by a variety of household devices and appliances. DiaCeph is an ideal home diagnostic tool to identify accidental reprogramming. There remains a pressing need for routine home patient monitoring and improvements in QA with respect to specifications and wider understanding of CNS shunts.
The DiaCeph Test meets five (5) areas of need in patients with CNS shunts:
1) Provides a real-time mobile method of documenting CNS shunt performance and shunt malfunction, as well as a tandem single in-office ICP tap;
2) Reveals complex intermittent shunt malfunction often with specificity, unobtainable thru other available diagnostic tests, via an elaborate "diagnostic decision tree;"
3) Enables accurate in-vivo comparison of shunts for pre-surgical shunt selection and planning, utilizing Aschoff et. al. bench test flow charts and mfr specs, rivaling information not available thru any diagnostic test, including 24-48 hour in-hospital ICP monitoring;
4) Serves as a standardized in-vivo assessment of CNS shunt outcomes, post discharge monitoring in ETV procedures, and comparative analysis of patient status over the long term; and
5) Enables the neurosurgeon along with the patient to more efficaciously determine the optimal opening pressure in programmable shunts, including, enabling a home determination in the event a programmable shunt should loose its setting.
Satellites and Shunts Have More in Common
The DiaCeph Monitoring System is integrates an interactive AI (artificial intelligence) design to monitor the neurological condition, hydrocephalus, in real time. In March 2007, DiaCeph was submitted to the American Electronics Association (AeA) 2007 High Technology Awards Contest, where it fared well with this Awards Presentation and 2007 Application.
CNS shunts involve fairly complicated consideration of fluid flows, gravitational forces, device opening pressures, performance measurements, and device failure. When CNS shunts fail to operate as intended, the patient's status will reflect changes in specific markers, or complaint parameters, that can be quantified and analyzed and made into a probable determination of the shunt's status. The DiaCeph Test also allows for in-vivo comparison of selected pressure settings in programmable shunts, and similarly, can be used in tandem with an ICP tap. A more detailed look at CNS shunt operation is explained through this Shunt Technology Perspectives presentation by Aschoff et. al. from the University of Heidelberg. Here is our recommended Codman programmable shunt calculator method for achieving the most physiological setting with Codman programmable shunts.
THE DIACEPH CNS SHUNT MONITORING SYSTEM
Patent No.
6,241,660 Of Counsel: Knobbe Martens Olson & Bear
The
Device
A method and computerized instrument for measuring CNS shunt performance in an individual with a hydrocephalus shunt by sampling specific clinical parameters as indicators of shunt performance, and intracranial pressure. Initial patient baseline monitoring is preferable, and where possible, to compare to incident and subsequent patient data all collected over a set time period. It is a palm device, but its method may also be constructed as a downloadable application for a mobile phone, where each employs several algorithms that translate non-invasive patient status data into diagnostic information. It is intended for patients who are conscious and four (4) years of age through late senior age, who are able to respond to queries, similar to a physician interview or standard hearing test. The results are stored with the patient’s history and default settings. Where the shunt may not be operating properly, the instrument further evaluates the data by comparison to earlier baseline and event data, and matches this to any of fourteen (14) known types of shunt malfunction.
Results would be available within the unit, via download to a PC or Internet web site, and via mobile phone uplinks to physicians for reviewing at remote locations. Test results would aid the physician in further diagnostic testing, surgical revision, and shunt and pressure selection. It functions as an advanced disease management program by compiling on-going detailed data on the patient's hydrocephalus status over the long term. It is intended for use by patients, family members, care givers, medical office staff, physicians, and researchers.
The
Concept and Current Standard
 The
concept for this product follows that shunt malfunction and changes in
intracranial pressure are accompanied by specific clinical complaints that may
vary by patient, but are diagnostic when analyzed appropriately. Its methodology
lies in real time assessment, first by baseline data and then at suspected
periods of shunt malfunction. Samples are also collected in series at set times
over a day. The device offers a reliable preliminary method of shunt evaluation,
with acceptable test sensitivity and specificity.
The
concept for this product follows that shunt malfunction and changes in
intracranial pressure are accompanied by specific clinical complaints that may
vary by patient, but are diagnostic when analyzed appropriately. Its methodology
lies in real time assessment, first by baseline data and then at suspected
periods of shunt malfunction. Samples are also collected in series at set times
over a day. The device offers a reliable preliminary method of shunt evaluation,
with acceptable test sensitivity and specificity.
A recent multi-center study by J. Kestle et. al., reported that CNS shunts overall had a 52% survival rate in the first two years post implantation. The study reported the Codman programmable shunt required re-programming in 70% of the cases during the first 6 months. A 1998 patient survey conducted by the Hydrocephalus Association of 422 respondents, in concert with the FDA’s Center for Devices and Radiologic Health (CDRH) and its 1999 STAMP Conference, found that the majority of respondents were deeply concerned about revisions, mechanical failures, infections, long term complications, and difficulty in assessing whether or not the shunt is functioning properly. Respondents were also concerned over quality of life issues, and 81% raised concerns that would be addressed by DiaCeph monitoring.
With respect to patient education, a July 2000 survey commissioned by the Medtronic Foundation reported 84% of Americans are taking more personal responsibility today in health matters than they did 10 years ago. Yet, 77% report today they do not have satisfactory control over their own health care. It is very common in patients implanted with programmable shunts (30-40 percent of population) for the devices to loose their correct setting. A 2005 paper, “The Billion Dollar a Year Cost of Hydrocephalus Treatment,” reported the average surgical shunt procedure now cost $35, 816. There are no accurate disability figures on hydrocephalus, which follows poor outcomes after shunting, but this figure is viewed as substantial.
Currently CT and MRI scanning currently are the staple
tests for determining shunt malfunction in the emergency room. These tests face limitations in that less than 50 percent will
demonstrate a measurable change in ventricular volume during malfunction, and
only after sufficient time and interruption of CSF outflow. Shunt
taps of ICP and drip rate currently offer some assessment, but are invasive and
only beneficial if the patient is obstructed at the time of the
exam. Patients are also examined for papilledema (increased ICP) and cranial nerve
changes, but again, there must be significant interruption in shunt CSF outflow
at time of exam. The clinician must factor each patient’s degree of
shunt dependency and shunt type.
Prospective Test
Applications
1.
Home and anytime documentation of intermittent and acute shunt malfunction.
2. Early home determination of accidental recalibration of programmable shunts.
3. Efficaciously determine the most optimal pressure setting in programmable shunts.
4. Enable medical office and school nurse evaluation of shunt function.
5. Post-discharge monitoring of patient status following CNS shunt and ETV procedures.
6. Improved shunt selection and pre-surgical planning prior to shunt revision.
7. Broadens and corroborates application on the single in-office ICP tap procedure.
8.
Evaluation of NPH and mild stage hydrocephalus, in tandem with Acetazolamide
Challenge Test.
9.
A patient management tool for the home setting, and an aid to daily activities
planning.
10.
A performance standard for in-vivo assessment of shunt systems in clinical
trials.
11.
Enable improvement in quality of life and independence in shunted teens and
adults.